group 20-35 years and then increased in ≥ 40 years group. Cataract is more typical in female when
contrasted with male as appeared in table: 1 by applying chi square test outcomes
were critical with
p value < 0.05.
Frequency of cataract in diabetic
patients with age groups shown in the table 2.
Table 3: Distribution of Cataract Type in Diabetics verses
Non-Diabetics
|
Type of
Cataract |
Diabetic |
Non-Diabetic |
|
PSCC |
43
(54.43%) |
3
(23.07%) |
|
Early
lenticular changes |
5
(6.32%) |
1 (7.69%) |
|
Nuclear
Cataract |
17
(21.51%) |
6 (46.15%) |
|
Cortical
Cataract |
14
(17.72%) |
3 (23.07%) |
|
Total |
79
(100.0%) |
13 (100.0%) |
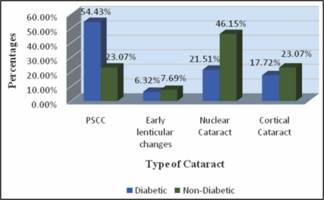
Graph 1: Type of Cataract in Diabetic and Non-Diabetic Patients.
Presence of diabetes and cataract is shown in the table 2
by applying chi square test result showed that Diabetes is significantly
associated with cataract with P value 0.001 at 5% margin of error with 95%
confidence interval. The outcomes were critical with
p value <0.05.
Table 3 shows; out of 99 diabetic patients, the most
common type of cataract was PSCC 43 (54.43%).
Out of 95 non-diabetic patients, the
most common type was nuclear cataract 6 (46.15%) as shown in table 3.
DISCUSSION
Duration of diabetes and age is a hazard factor for
advancement of cataract in diabetic patients. Charles et al. examine
in 2003 in which normal term of diabetes was 7 years and the time of diagnosis
was 46.5 years.14 While
in present examination, the span of diabetes was 6-7 years. Although in present
study age was classified into two groups 20-35 &36-50 years. Results showed
that subjects in 20-35 years, 6 (9.1%) had cataract. While subjects in 36-50
years, 86 (67.2%) were presented with cataract including diabetic and non-diabetic.
Cataract was more in age between 36-50 years. Thus, result of both studies are
almost equal.
In 2003 Charles et al. reported prevalence of cataract
44.9% in West African type 2 diabetic patients which is almost half as compared
to in our population14.In present study diabetic cataract was
present in 79 (85.9%) and absent in 20 (19.6%). Although in non-diabetic
patients cataract was present in 13 (14.1%) and absent in 82 (80.4%) patients. Diabetes
is the major risk factor for cataract.
When considering the higher prevalence of diabetes
mellitus in females, it follows that the incidence of diabetic cataract would
be higher in females than male. Sung et al.in 2006 reported that two groups of
diabetic patients, one was control group and the other was cataract group. The
author (s) concluded that females were more common in cataract group than
control group.12 Similar
to present study in which prevalence of diabetes and cataract was more in
females than male. Out of 194 patients 63 (52.94%) females and 29 (38.66) male
were presented with cataract. In term of relationship between diabetes and
gender, the increased incidence of diabetic cataract were appeared in females.
In 2012 Eydis conducted study on prevalence of cataract in
a population with and without type 2 diabetes mellitus. According to author 274
patients were diagnosed with diabetes and 256 controlled. Three types of
cataract was observed 65.5% cortical, 42.5% PSCC and 48% nuclear cataract in
type 2 diabetes15.Similarly to compare most recent studies, Patricia
et al. conducted study in 2017 on pre-senile cataract in diabetic Patients. The
hypothesis of Patricia was a cortical cataract is more common in diabetic
population. Patricia looked at the discoveries of best quality level LOCS III
(lens opacity classification system III) with scheimpflug target measures in a
presenile population. Author(s) concluded that out of 43 diabetic patients
88.4% were having sub capsular cataract, 52.3% cortical and 7% nuclear cataract
that is twice as compared to present study16.While in 2010 Rajiv
Raman concluded that among the monotype cataracts, CC was the most common
subtype in patients with type 2 DM (15.1%). In the mixed cataracts, the
combination of NC, CC, and PSC was the most common (19.5%)17.
Results of present study shows for diabetic as well as for
non-diabetic patients. It shows significant association between diabetes and
PSCC. In this study 43 (54.43%) PSCC, 14 (17.72%) cortical and 17 (21.51%)
nuclear cataract in diabetic patients that was definitely higher than previous
study. While in non-diabetic patients 3 (23.07%) were present with PSCC, 1
(7.69%) present with early lenticular changes, 6 (46.15%) present with nuclear
cataract and cortical cataract was 3 (23.07%).Subsequently, early improvement
of pharmacological and careful methods for cataract anticipation ought to be
one of the fundamental needs for future cataract examine. These intercessions
must encouraging to overcome the expanding
pervasiveness of cataract in diabetic patients18.
Currently the only available
treatment for disease is surgical removal of opaque lens and followed by
replacement with synthetic implants. Efforts have been taken to explore the
traditional medicine to delay and retard the progression of cataract. Several
numbers of plants and synthetic compounds has been reported to possess
anti-cataract activity.19Success
rate of cataracts surgery, without serious complications and improved vision is
possible with the advanced surgical procedure and with the aid of equipment’s.20 However, most common side
effects reported in the post-surgical treatment was inflammatory reaction and
cystoid macular oedema21.
CONCLUSION
Cataract was present 79% in defined
population. This study shows that there is high frequency of cataract in
diabetic patients which can be avoided its consequences delayed if they are
timely referred to ophthalmologist to diagnose and manage early for better
visual outcomes.
ACKNOWLEDGMENT
I paid my tributes and thank to Miss
Tayyaba Rahat for encouragement and support from the initial to the final level
of this work. Special thank for helping me in statistical analysis.
Conflict
of Interest
Approved by ethical committee &
IRB of institute.
Funding
Sources
Self-funded Hospital data was used.
Authors
Affiliation
Kiran Aslam
Bsc.(Hons) Optometery & Orthoptics
FMH College of Medicine &
Dentistry
Dr. Muhammad Sufyan Aneeq Ansari
Assistant Professor of Ophthalmology
Fatima Memorial Hospital Lahore
Imran Khalid
Orthoptist BSVS, M.phil (Sch), CRCP
Services Hospital Lahore
Dr. Khurram Nafees
Assistant Professor of Ophthalmology,
Fatima Memorial Hospital Lahore
Author’s
Contribution
Kiran Aslam
Substantial Contribution in
conception, designing, acquisition, analysis or interpretation of data.
Dr. Muhammad Sufyan Aneeq Ansari
Final approval of manuscript.
Imran Khalid
Manuscript drafting & revision
for intellectual content.
Dr. Khurram Nafees
Contribution in conception &
designing of manuscript.
REFERENCES
1.
Kanski
JJ. Clinical ophthalmology. 8th ed. Vol. 1. NewSouth Wales,
Australia: Butterworths, 1989: 270-300.
2.
Thomson William. Diseases of
The Eye. 4th ed. Vol. 1. S.l: Hansebooks, 2016: 110-114.
3.
Lathika
V, Ajith T. Association of grade of cataract
with duration of diabetes, age and gender in patients with type II diabetes
mellitus. International Journal of Advances in Medicine, 2016; (1): 304–8.
4.
Gupta
S, Selvan V, Agrawal S, Saxena R. Advances in pharmacological
strategies for the prevention of cataract development. Indian Journal of
Ophthalmology, 2009, 57(3):175.
5.
Open Access Research
Prevalence and causes of visual... [Internet].[cited
2018Oct14].Availablefrom:https://bmjopen.bmj.com/content/bmjopen/8/3/e018894.full.pdf
6.
Negahban
K, Chern K. Cataracts associated with systemic
disorders and syndromes. Current Opinion in Ophthalmology, 2002; 13(6):419–22.
7.
Patel
PM, Jivani N, Malaviya S, Gohil T, Bhalodia Y.
Cataract: A major secondary diabetic complication. International Current
Pharmaceutical Journal, 2012; Mar 1(7): 3-57.
8.
Jatoi
SM. Clinical ophthalmology. 5th ed. Vol. 1. Karachi,,
Pakistan: Paramount Books; 2013: 269-272.
9.
Dineen
B, Bourne RRA, Jadoon Z, Shah SP, Khan MA, Foster A, et al.
Causes of blindness and visual impairment in Pakistan. The Pakistan national
blindness and visual impairment survey. British Journal of Ophthalmology, 2007;
91(8):1005–10.
10.
Jadoon
Z, Shah S, Bourne R, Dineen B, Khan M, Gilbert C et al.
Cataract prevalence, cataract surgical coverage and barriers to uptake of
cataract surgical services in Pakistan: the Pakistan National Blindness and
Visual Impairment Survey. British Journal of Ophthalmology, 2007;
91(10):1269-1273.
11.
Marathe
PH, GAOHX, Close KL. American Diabetes
Association Standards of Medical Care in Diabetes2017.Journal of Diabetes, 2017;
9(4):320–4.
12.
Kim
SI, Kim SJ. Prevalence and Risk Factors for Cataracts
in Persons with Type 2 Diabetes Mellitus. Korean Journal of Ophthalmology, 2006;
20(4):201.
13.
Visual Outcome of Cataract
Surgery after Phacoemulsification [Internet]. [Cited 2018Oct15]. Available
from: http://www.pjo.com.pk/33/4/9.
Sanaullah - MM31Dec.pdf
14. Rotimi C,
Daniel H, Zhou J, et al. Prevalence and determinants of diabetic
retinopathy and cataracts in West African type 2 diabetes patients. Ethn Dis 2003; 13(2 Suppl 2): S110-7. 22
15.
Olafsdottir
E, Andersson DKG, Stefánsson E. The prevalence of cataract in
a population with and without type 2 diabetes mellitus. ActaOphthalmologica.2011;
90(4):334–40.
16.
Kyselova
Z, Stefek M, Bauer V. Pharmacological prevention
of diabetic cataract. Journal of Diabetes and its Complications, 2004;
18(2):129–40.
17.
Raman
R, Pal SS, Adams JSK, Rani PK, Vaitheeswaran K, Sharma T.
Prevalence and Risk Factors for Cataract in Diabetes: Sankara Nethralaya
Diabetic Retinopathy Epidemiology and Molecular Genetics Study, Report No. 17.
Invest Opthalmol & Vis Sci. 2010; 51(12):6253.
18.
Rooban
BN, Sasikala V, Sahasranamam V, Abraham A.
Vitexnegundo Modulates Selenite-Induced Opacification and Cataractogensis in
Rat Pups. Biological Trace Element Research, 2010; 138(1-3):282–92.
19.
Dowler
JG, Hykin PG, Hamilton AM. Phacoemulsification versus
extracapsular cataract extraction in patients with diabetes. Ophthalmol. 2000;
107(3):457-62. 23.
20.
Prokofyeva
E, Wegener A, Zrenner E. CataractprevalenceandpreventioninEurope:aliteraturereview.ActaOphthalmologica.2012;
91(5):395–405.
21.
Gus
PI, Zelanis S, Marinho D, Kunzler AL, Nicola F, Folle H, et al.
Pre-SenileCataract in Diabetic Patients: Prevalence and Early Diagnosis.
Journal of Clinical Trials, 2017; 07(02): 44-67.